Intermittent Abdominal Pain Week 3 Discussion Essay
Intermittent Abdominal Pain Week 3 Discussion Essay
Intermittent Abdominal Pain Week 3 Discussion Essay
Today, an 18-year-old Caucasian female appears with intermittent stomach pain. She also has a low-grade fever, cramps, and diarrhea. She has also lost her appetite. She acknowledges smoking 1/2 PPD for two years. Denies using illegal drugs or alcohol and reports a Crohn’s disease history.
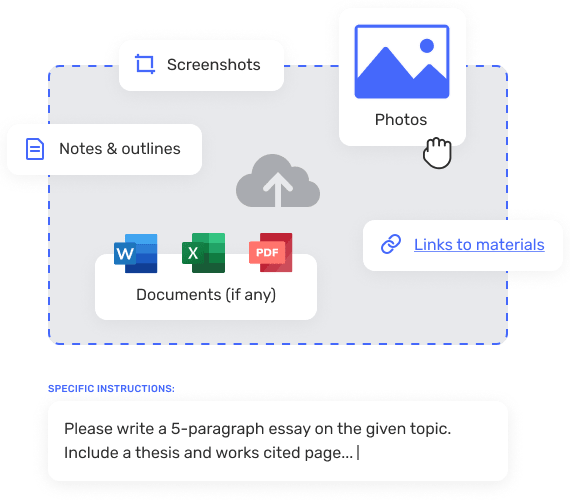
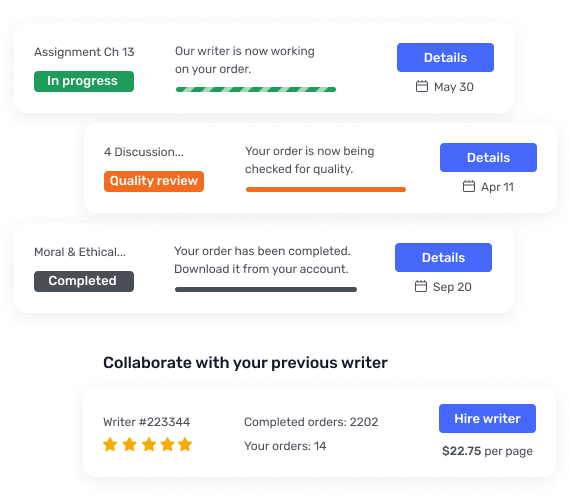
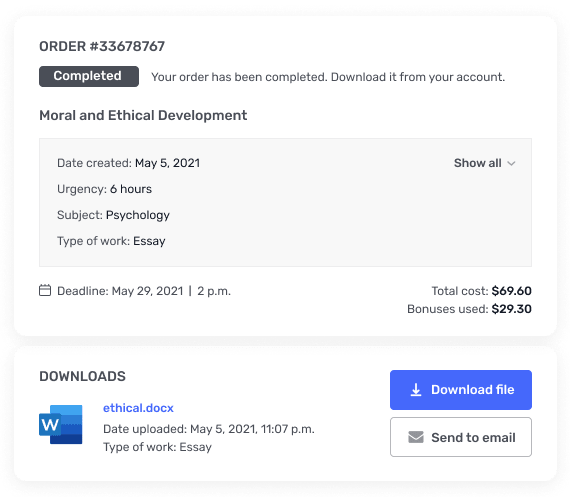
ORDER A CUSTOM PAPER NOW
Differential Diagnosis
The top differentials I would consider include Crohn’s disease, ulcerative colitis, and appendicitis. The inflammatory bowel diseases Crohn’s disease (CD) and ulcerative colitis (UC) have an immunological basis (Ranasinghe & Hsu, 2022). The trajectory of Crohn’s disease is one of remission and relapse. Typical symptoms of Crohn’s disease flare-ups include stomach discomfort, bloating, diarrhea, fever, weight loss, and anemia. Many of the manifestations can be seen in the patient. Ulcerative colitis is an inflammation of the colon that has no known cause. Bloody diarrhea, whether it contains mucus or not, is the predominant sign. Depending on how far the illness has spread and how bad it is, one may also have tenesmus, malaise, abdominal pain, weight loss, and fever (Lynch & Hsu, 2023). The condition usually worsens over time, and people with it often go through periods of remission followed by relapses. When the vermiform appendix gets inflamed, this is called appendicitis. According to research, anorexia and periumbilical pain are common symptoms of appendicitis, and they frequently precede right lower quadrant pain, nausea, vomiting, fever, and other symptoms (Echevarria et al., 2023). Crohn’s disease is, therefore, the presumptive diagnosis.
Focused Physical Examination
It would be useful for the patient with a suspected Crohn’s disease flare-up to have several targeted physical exam results. After visually inspecting the patient’s abdomen, all four quadrants should be auscultated to listen for any altered bowel sounds that might indicate obstruction. After that, the abdomen should be palpated to check for organomegaly, ascites, rebound pain, or distention (Ranasinghe & Hsu, 2022). All patients require a perineum exam. Skin tags, fistulas, scars, ulcers, and abscesses could all be seen during the examination.
Diagnostic testing to confirm the diagnosis
A thorough investigation is required for diagnosis confirmation. Infections can be ruled out by stool tests for culture, ovum and parasites, C. difficile toxins, leukocyte count, and calprotectin, which can identify active Crohn’s disease. It is possible to differentiate between Crohn’s disease and ulcerative colitis using blood tests such as the CBC, metabolic panel, ANCA, and ASCA. CRP or ESR indicates how severe the inflammation is (Kedia et al., 2019; Ranasinghe & Hsu, 2022). While plain X-rays can reveal intestinal obstruction, imaging techniques like CT scan/MRE of small bowel follow-through and VCE can see the afflicted areas.
Evidence-based treatment Approach
Crohn’s disease should be treated with a multidisciplinary approach based on the patient’s needs. Evidence-based treatment guidelines suggest that people with Crohn’s disease may need to take medicine and change their lifestyle. Anti-inflammatory drugs like aminosalicylates or corticosteroids can help reduce inflammation in the bowel (Ranasinghe & Hsu, 2022). Immune system suppressors like azathioprine or methotrexate stop the immune system from attacking the bowel. Anti-TNF drugs like infliximab, adalimumab, and golimumab block TNF to stop it from causing inflammation (Ranasinghe & Hsu, 2022). Nutritional support, such as a low-residue or elemental diet, is required to give the bowel time to recover. Smoking cessation and stress management are two lifestyle changes that can help to lessen flare-ups.
References
Echevarria†, S., Rauf†, F., Hussain†, N., Zaka, H., Farwa, U. -, Ahsan, N., Broomfield, A., Akbar, A., & Khawaja, U. A. (2023). Typical and atypical presentations of appendicitis and their implications for diagnosis and treatment: A literature review. Cureus. https://doi.org/10.7759/cureus.37024
Jones, M. W., Lopez, R. A., & Deppen, J. G. (2022). Appendicitis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK493193/#:~:text=Appendicitis%20is%20the%20inflammation%20of
Kedia, S., Das, P., Madhusudhan, K. S., Dattagupta, S., Sharma, R., Sahni, P., Makharia, G., & Ahuja, V. (2019). Differentiating Crohn’s disease from intestinal tuberculosis. World Journal of Gastroenterology, 25(4), 418–432. https://doi.org/10.3748/wjg.v25.i4.418
Lynch, W. D., & Hsu, R. (2023). Ulcerative colitis. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459282/#:~:text=Introduction-
Ranasinghe, I. R., & Hsu, R. (2022, May 15). Crohn disease. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK436021/
ORDER A CUSTOM PAPER NOW
An 18-year-old white female presents to your clinic today with a 2-week history of intermittent abdominal pain. She also is positive for periodic cramping and diarrhea as well as low grade fever. She also notes reduced appetite. She notes that She admits smoking ½ PPD for the last 2 years. Denies any illegal drug or alcohol use. Does note a positive history of Crohn’s Disease. Based on the information provided answer the following questions:
What are the top 3 differentials you would consider with the presumptive final diagnosis listed first?
What focused physical exam findings would be beneficial to know?
What diagnostic testing needs completed if any to confirm diagnosis?
Using evidence based treatment guidelines note a treatment plan.