Assignment: Evidence-Based Project, Part 3: Critical Appraisal of Research
Assignment: Evidence-Based Project, Part 3: Critical Appraisal of Research
|
Evidence-Based Project, Part 3A & B: Critical Appraisal of Research
NURS – 6052: Essentials of Evidence-Based Practice
Evaluation Table
| Full APA formatted citation of the selected article. | Article #1 | Article #2 | Article #3 | Article #4 |
| Burja, S., Belec, T., Bizjak, N., Mori, J., Markota, A., & Sinkovič, A. (2018). Efficacy of a bundle approach in preventing the incidence of ventilator-associated pneumonia ( VAP ). Bosnia Journal of Basic Medical Science, 18(1), 105–109.
|
De Neef, M., Bakker, L., Dijkstra, S., Raymakers-Janssen, P., Vileito, A., & Ista, E. (2019). Effectiveness of a ventilator care bundle to prevent ventilator-associated pneumonia at the PICU: A systematic review and meta-analysis. Pediatric Critical Care Medicine, 20(5), 474–480. https://doi.org/10.1097/PCC.0000000000001862
|
Mahmoodpoor, A., Hamishehkar, H., Hamidi, M., Shadvar, K., Sanaie, S., Golzari, S. E., Khan, Z. H., & Nader, N. D. (2017). A prospective randomized trial of tapered-cuff endotracheal tubes with intermittent subglottic suctioning in preventing ventilator-associated pneumonia in critically ill patients. Journal of Critical Care, 38, 152–156. https://doi.org/10.1016/j.jcrc.2016.11.007
|
Triamvisit, S., Wongprasert, W., Puttima, C., Chiangmai, M. N., Thienjindakul, N., Rodkul, L., & Jetjumnong, C. (2021). Effect of a modified care bundle for prevention of ventilator-associated pneumonia in critically ill neurosurgical patients. Acute and Critical Care, 36(4), 294–299. https://doi.org/10.4266/acc.2021.00983
|
|
| Evidence Level *
(I, II, or III)
|
III: A retrospective analysis in which data gathering heralded the formulation of the PICO (population, intervention, comparison, outcomes) question (The Johns Hopkins Hospital/Johns Hopkins University, n.d.). | II: A systematic review with meta-analysis of a combination of randomized controlled trials (RCTs) and quasi-experimental studies (The Johns Hopkins Hospital/Johns Hopkins University, n.d.) Assignment: Evidence-Based Project, Part 3: Critical Appraisal of Research | I: A well-designed RCT | II: A well-designed prospective cohort study |
| Conceptual Framework
Describe the theoretical basis for the study (If there is no one mentioned in the article, say that here).**
|
None |
None |
None
|
None |
| Design/Method
Describe the design and how the study was carried out (In detail, including inclusion/exclusion criteria). |
The study involved a retrospective analysis of data of patients admitted to a hospital intensive care unit (ICU) to determine the effectiveness of ventilator-associated pneumonia (VAP) care bundle in decreasing the occurrence of VAP cases. The inclusion criteria include all adult patients in ICU irrespective of the origin department; mechanically ventilated with an endotracheal tube (ETT); and the absence or presence of VAP | The investigation involved a systematic review and meta-analysis of RCTs and quasi-experimental studies to examine the efficacy of ventilator bundle in severely ill pediatrics. It involved a search of five electronic databases, including Web-of-Science, OvidSP, PubMed, Embase, and Cochrane Library RCTs on the application of VAP care bundle to decrease the odds of VAP in mechanically ventilated pediatrics. Studies were included in the meta-analysis if they were RCTs, non-randomized studies, or interrupted time series; the intervention was VAP bundle in pediatric ICU, multicomponent approach, or quality improvement with the principal aim of decreasing VAP frequencies, and the control was usual care or an element of the ventilator care bundle. Assignment: Evidence-Based Project, Part 3: Critical Appraisal of Research | The study involved a prospective RCT, where participants were randomly allocated to either conventional high-volume low-pressure ETT (group C) or intubation with TaperGuard tubes (group E). The groups were evaluated to determine the efficacy of the use of TapeGuard in subglottic suctioning in reducing VAP incidences.
The patients were selected if they were aged between 18 and 80 years, requiring assisted ventilation for ≥72 hours with ETT. |
The authors adopted a prospective cohort research design, where adults aged ≥18 years with neurological conditions were recruited and observed from November 2018 -June 2020 after the implementation of a modified VAP bundle. The modified bundle involved extending the time of discontinuous cuff pressure monitoring to every 4-hours 6 times.
The inclusion criteria included adult patients in the neurological department aged ≥18 years, mechanically ventilated and intubated for ≥24 hours, no indications of VAP, not being end-of-life patients and no fractured cervical spine or contraindication for head-of-bed elevation. |
| Sample/Setting
The number and characteristics of patients, attrition rate, etc. |
The study was conducted at the ICU of the University Medical Centre Maribor, Slovenia.
A total of n = 129 patients were included in the study, including n = 74 artificially ventilated patients with ETT post-VAP bundle implementation (VAP-B), with a mean age of 64.8 ± 13.7 years and 62.1% males, and n = 55 artificially ventilated patients with ETT pre-VAP bundle introduction (no-VAP-B) with a mean age of 67.8 ± 14.5 years and 45.5% females.
The posthoc analysis of retrospective data includes no report of participant dropouts or loss to follow-up in the study. |
A total of n = 11 studies that met the eligibility benchmark were included in the review.
Two of the studies involve multi-center assessments and the remaining nine were conducted in a single center. One study had an interrupted time series design while ten involved pre-post-interventional frameworks.
|
A total of n = 276 patients participated in the RCT, including n = 138 in group E and 138 in group C.
The patients were aged between 18 – 80 years, requiring assisted ventilation for ≥72 hours with ETT. None was lost to follow-up in either cohort Mean age 54 years |
A total of n = 291 neurological patients, including n = 145 in the treatment group and n = 146 in the matched cohort. The patients had a mean Glasgow coma score of 7.80 at baseline with no significant differences in gender between groups. |
| Major Variables Studied
List and define dependent and independent variables |
Dependent variables:
Independent variables:
|
Dependent variables:
Independent variables:
|
Dependent variables:
Independent variables
|
Dependent variables:
Independent variable:
|
| Measurement
Identify primary statistics used to answer clinical questions (You need to list the actual tests done). |
VAP-B group was compared to the no-VAP-B cohort. Unpaired t-test was used to match means between the two cohorts and Fisher’s exact test for categorical variables. A 2-sided p-value <0.05 was regarded as statistically significant. | All the data from individual studies were pooled in the meta-analysis using a DerSimonian and Laird random-effects model.
Cochrane Q test and the inconsistency index (I2) was used to test heterogeneity in the studies [High I2 >75%, Moderate I2= 50 – 75%, and Low I2 = 25 – 50%]. |
Kolmogorov-Smirnov battery was performed to test the normality of distribution for continuous variables.
Chi-square (X2) was used to compare the efficacy of the intervention versus usual care in decreasing VAP incidences |
Quantitative data were reported as mean ± standard deviation, percentage, and frequencies.
Fischer’s exact test was used to statistically compare the dependent variables between cohorts.
Mann Whitney U-test was applied to compare the length of mechanical ventilation. |
| Data Analysis Statistical or
Qualitative findings (You need to enter the actual numbers determined by the statistical tests or qualitative data). |
The results showed no significant disparity observed between VAP-B and no-VAP-B groups in the frequency of the use of ETTs [58.1% versus 60%, p = 0.05]. There were no statistically substantial differences between VAP-B and no-VAP-B groups in hospital mortality [49.3% versus 48.2%, p>0.99] or ICU mortality [34.7% versus 41.1%, p =0.47]. The length of hospital stay [11.3 ± 10.9 days versus 11.7 ± 9.5 days, p = 0.85] and duration of artificial ventilation [8.4 ± 7.3 days versus 9.1 ± 7.8 days, p = 0.55] were comparatively similar in both cohorts. The incidence rates of VAP differed between VAP-B and no-VAP-B cohorts [25.7% versus 41.8%] but the difference was not statistically substantial (p = 0.06); however, a significantly lower rate of late VAP was noted in the VAP-B group. | 11 articles that met the eligibility benchmark were identified and meta-synthesized.
The baseline incidence of VAP ranged from 3.9 – 28.3/1000 ventilator days, which dropped to 4.6/1000 ventilator days after the enforcement of the ventilator care bundle, with the pooled incident risk ratio (IRR) in line with the efficacy of the ventilator bundle in diminishing VAP cases [IRR = 0.45; 95% CI, 0.33–0.60; I2 = 55%p < 0.0001]. Adherence to the elements of the ventilator bundle was high for head-of-bed elevation and low for evaluation of readiness to extubate and interruption of sedation. |
There was no statistically substantial disparity between groups E and C concerning VAP risk factors, P02, and demographic features at the baseline.
The mean cuff pressure in the treatment cohort was substantially less than in the control cohort [P<0.001]
The incidence of VAP/1000 ventilator days was substantially less in the treatment group than in the control cohort [P = 0.015]. The TaperGuard tubes with alternating subglottic secretion drainage had no substantial changes in VAP-related mortality. |
The frequency of VAP was significantly low in the cohort group than in the matched group [0.88/1,000
vs. 6.84/1,000 ventilator days, P=0.036]. However, the intervention did not affect the length of ICU stay and the rates of re-intubation. |
| Findings and Recommendations
General findings and recommendations of the research |
The study demonstrated that the implementation of a ventilator bundle that focuses on ETT with subglottic suction decreases the odds of VAP, with a significant effect on late VAP cases. Thus, a VAP care bundle involving the use of ETT with subglottic suction every 4 hours, oral care with chlorhexidine, head-of-bed elevation, maintaining endotracheal cuff pressure at 25 cm H20, and daily evaluation for extubation, is recommended in ICU to mitigate VAP. | The implementation of a VAP care bundle can facilitate the reduction of VAP among severely sick pediatrics; however, adherence to the bundle’s elements is fundamental to its effectiveness. | Overall, the findings of the trial showed that the use of TaperGuard in ETT subglottic suctioning was superior to the traditional ETT subglottic suction in decreasing the occurrence of VAP cases among severely ill adults patients. | The modified VAP bundle has higher or comparable effectiveness in decreasing the occurrence of VAP than the standard VAP bundle. |
| Appraisal and Study Quality
Describe the general worth of this research to practice.
What are the strengths and limitations of the study?
What are the risks associated with the implementation of the suggested practices or processes detailed in the research?
What is the feasibility of use in your practice? |
The strength of the study is the aspect that the authors asked a focused clinical question with a clear population of interest, intervention, comparison, and target outcomes.
However, the evaluation of the efficacy of clinical interventions calls for the use of prospective study designs (Emptage et al., 2018). Thus, the validity of the findings of Burja et al. (2018) study is threatened by the retrospective nature of the research design.
Besides, the investigation was conducted in a single setting, thus, the results might not be generalizable to other hospitals.
Nonetheless, the findings are supported by meta-analyses and randomized clinical trials making the recommendations feasible in my clinical practice. |
While the authors cited that they targeted RCTs and non-RCTs, 90% were pre-post interventional studies. The participants were not randomly assigned to intervention and control groups, which enhances the risk of bias and decreases the validity of the findings.
The strengths of the meta-analysis are the use of pooled ratio to compute the incidence of VAP cases and asking a focused clinical question However, the included studies did not include a single RCT and differed substantially concerning the country of publication, baseline measurements, population characteristics, and study design. Besides, high clinical and methodological heterogeneity was observed in the studies resulting in a moderate inconsistency in the ventilator bundles. The results are applicable in my clinical practice in decreasing the odds of VAP among children and infants receiving mechanical ventilation in PICU. |
The trial authors asked a focused clinical question and used computer software to generate random numbers for the randomization of the participants into the treatment groups. They also provided the study protocol, applied a narrow confidence interval which demonstrates a significant difference between treatment and control cohorts, and there was no participant loss to follow-up. Besides, the research assistants helping in data collection were blinded to minimize bias and maximize the validity of the findings
All the above factors addressed potential bias, thereby enhancing the reliability and validity of findings. However, the trial was conducted at a single center, which limits the extrapolation of the findings.
There are no explicit risks associated with the implementation of the recommended TaperGuard in ETT subglottic suctioning alongside all the elements of the ventilator bundle.
Currently, our hospital relies on the conventional ETT with subglottic suctioning; however, given the superiority of the proposed TaperGuard tubes, it is feasible to implement it to reduce the odds of VAP. The TaperGuard tubes are not only cost-effective but also user-friendly. |
The study results’ validity is enhanced by the prospective nature of the research design. Besides, the authors asked a focused clinical question; however, the historical cohort might have been subjected to non-compliance and selection bias.
There are no known risks associated with the modified VAP bundle; therefore, it is safe for implementation in local settings.
Besides, as recommended by the study authors, the modified ventilator bundle can serve as an alternative to continuous cuff pressure monitoring as it is not only effective in reducing the odds of VAP but also cost-effective (Triamvisit et al., 2021). |
|
Key findings
|
The enforcement of the ventilator bundle is allied to a downward trend towards a lower occurrence of VAP and a substantially lower incidence of late VAP. | The implementation of and adherence to all the elements of the VAP care bundle can expedite the decline in VAP incidences among severely sick pediatrics | TaperGuard tubes used in ETT subglottic suctioning significantly reduced the occurrence of VAP when matched with traditional tubes. Nonetheless, the tubes did not have any impact on VAP-associated mortality. | The modified ventilator bundle includes adjustment of two elements; oral care and ET cuff pressure monitoring. The prospective cohort study revealed that increasing the length and frequency of ET cuff pressure monitoring prevents microaspiration associated with underinflation (Khan et al., 2017). |
|
Outcomes
|
|
|
|
|
| General Notes/Comments | The implementation and sustained use of the VAP bundle decreases the frequency of VAP cases among critically ill adults.
|
Adherence to the elements of the ventilator care bundle is at the crux of successful implementation and effectiveness of ventilator bundles in decreasing the odds of VAP among seriously ill pediatrics. | The utilization of TaperGuard tubes with discontinuous subglottic drainage substantially reduces the risk of VAP among critically ill patients. | There is a need to modify the VAP bundle accordingly depending on the types of the critically-ill patient population |
Part 3B: Critical Appraisal of Research
The four critically appraised articles included studies, a retrospective study (Burja et al., 2018), a systematic review (De Neef et al., 2019), an RCT (Mahmoodpoor et al., 2017), and a prospective cohort study (Triamvisit et al., 2021). All the articles’ authors asked focused clinical questions, with a clearly defined population of interest, interventions, comparator, and target outcomes. The PICOT question my project seeks to answer states: is the ventilator bundle superior to usual care in reducing VAP cases among mechanically ventilated and/or intubated patients in ICU six months after implementation? The PICOT question focuses on the evaluation of a clinical intervention, which necessitates the support from well-designed high-level empirical evidence, such as RCTs, systematic reviews with meta-analysis of RCTs, and prospective cohort studies (Emptage et al., 2018). From the four critically appraised articles, the retrospective nature of Burja et al. (2018) study threatens the validity of its findings, while the inclusion of pre-post interventional studies in the De Neef et al. (2019) meta-analysis diminished the cogency and applicability of the results Assignment: Evidence-Based Project, Part 3: Critical Appraisal of Research.
The RCT study offers high-quality findings due to the well-designed procedures. The trial authors asked a focused clinical query using the PICO framework, which involved seeking to determine whether the use of TaperGuard EVAC tubes in subglottic drainage is superior to conventional tubes in reducing the incidence of VAP (Mahmoodpoor et al., 2017). The author used a computer-generated randomizer to randomly assign the participants into treatment cohorts, blinded the research assistant involved in data gathering, and properly accounted for all the patients who entered the trial at its conclusion thereby decreasing the odds of attrition bias (Mansournia et al., 2017). The random allocation of the patients to the treatment cohorts decreased the odds of inadvertent or deliberate biases that might have diminished the cogency of the RCT results (Mittlböck, 2018). Nonetheless, while the patients in Mahmoodpoor et al. (2017) RCT were analyzed in their allocated intervention groups, the authors failed to provide a clear description of the intention-to-treat procedure. Besides, the trial authors based their sample size determination on previous studies reporting the incidence rate of 9 – 27 % for VAP in intubated patients using a power of 89% with α = .05, and an expected failure rate for experimental subjects of 0.135 (Mahmoodpoor et al., 2017). All the above features enhance the validity of the trial findings; however, conducting the study at a single center reduces the likelihood of generalizing the results.
References
Burja, S., Belec, T., Bizjak, N., Mori, J., Markota, A., & Sinkovič, A. (2018). Efficacy of a bundle approach in preventing the incidence of ventilator-associated pneumonia ( VAP ). Bosnia Journal of Basic Medical Science, 18(1), 105–109.
De Neef, M., Bakker, L., Dijkstra, S., Raymakers-Janssen, P., Vileito, A., & Ista, E. (2019). Effectiveness of a ventilator care bundle to prevent ventilator-associated pneumonia at the PICU: A systematic review and meta-analysis. Pediatric Critical Care Medicine, 20(5), 474–480. https://doi.org/10.1097/PCC.0000000000001862
Emptage, N., Koster, M., Schottinger, J., & Petitti, D. (2018). Critical appraisal of clinical studies: An example from computed tomography screening for lung cancer. The Permanente Journal, 11(2), 81–85. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3057745/
Khan, M., Khokar, R., Qureshi, S., Al Zahrani, T., Aqil, M., & Shiraz, M. (2017). Measurement of endotracheal tube cuff pressure: Instrumental versus conventional method. Saudi Journal of Anaesthesia, 10(4), 428. https://doi.org/10.4103/1658-354X.179113
Mahmoodpoor, A., Hamishehkar, H., Hamidi, M., Shadvar, K., Sanaie, S., Golzari, S. E., Khan, Z. H., & Nader, N. D. (2017). A prospective randomized trial of tapered-cuff endotracheal tubes with intermittent subglottic suctioning in preventing ventilator-associated pneumonia in critically ill patients. Journal of Critical Care, 38, 152–156. https://doi.org/10.1016/j.jcrc.2016.11.007
Mansournia, M. A., Higgins, J. P. T., Sterne, J. A. C., & Hernán, M. A. (2017). Biases in randomized trials. Epidemiology, 28(1), 54–59. https://doi.org/10.1097/EDE.0000000000000564
Mittlböck, M. (2018). Critical appraisal of randomized clinical trials: Can we have faith in the conclusions? Breast Care, 3(5), 341–346. https://doi.org/10.1159/000157168
The Johns Hopkins Hospital/Johns Hopkins University. (n.d.). Johns Hopkins Nursing Evidence-Based Practice Appendix C : Evidence Level and Quality Guide. https://www.hopkinsmedicine.org/evidence-based-practice/_docs/appendix_c_evidence_level_quality_guide.pdf
Triamvisit, S., Wongprasert, W., Puttima, C., Chiangmai, M. N., Thienjindakul, N., Rodkul, L., & Jetjumnong, C. (2021). Effect of a modified care bundle for prevention of ventilator-associated pneumonia in critically ill neurosurgical patients. Acute and Critical Care, 36(4), 294–299. https://doi.org/10.4266/acc.2021.00983
Assignment: Evidence-Based Project, Part 3: Critical Appraisal of Research
Realtors rely on detailed property appraisals—conducted using appraisal tools—to assign market values to houses and other properties. These values are then presented to buyers and sellers to set prices and initiate offers.
Research appraisal is not that different. The critical appraisal process utilizes formal appraisal tools to assess the results of research to determine value to the context at hand. Evidence-based practitioners often present these findings to make the case for specific courses of action Assignment: Evidence-Based Project, Part 3: Critical Appraisal of Research.
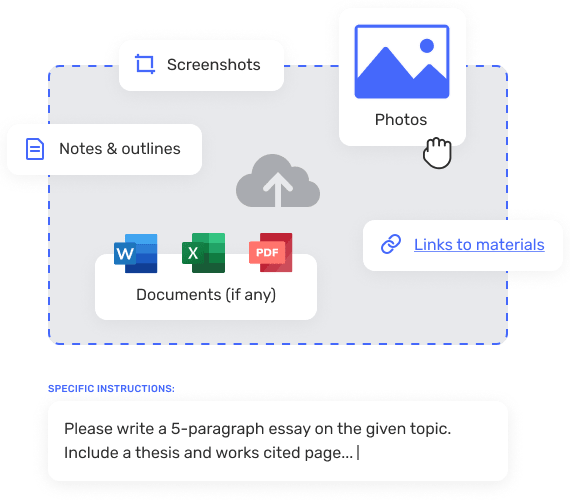
In this Assignment, you will use an appraisal tool to conduct a critical appraisal of published research. You will then present the results of your efforts.
To Prepare:
- Reflect on the four peer-reviewed articles you selected in Module 2 and the four systematic reviews (or other filtered high- level evidence) you selected in Module 3.
- Reflect on the four peer-reviewed articles you selected in Module 2 and analyzed in Module 3.
- Review and download the Critical Appraisal Tool Worksheet Template provided in the Resources.
The Assignment (Evidence-Based Project)
Part 3A: Critical Appraisal of Research
Conduct a critical appraisal of the four peer-reviewed articles you selected by completing the Evaluation Table within the Critical Appraisal Tool Worksheet Template. Choose a total of four peer- reviewed articles that you selected related to your clinical topic of interest in Module 2 and Module 3.
Note: You can choose any combination of articles from Modules 2 and 3 for your Critical Appraisal. For example, you may choose two unfiltered research articles from Module 2 and two filtered research articles (systematic reviews) from Module 3 or one article from Module 2 and three articles from Module 3. You can choose any combination of articles from the prior Module Assignments as long as both modules and types of studies are represented.
Part 3B: Critical Appraisal of Research
Based on your appraisal, in a 1-2-page critical appraisal, suggest a best practice that emerges from the research you reviewed. Briefly explain the best practice, justifying your proposal with APA citations of the research. Assignment: Evidence-Based Project, Part 3: Critical Appraisal of Research