Emerging Technology Brief NUR 514
Emerging Technology Brief NUR 514
Emerging Technology Brief
In order to improve patient outcomes, modern health care places a strong emphasis on the patient. Health care professionals must store and secure the accessible data in order to appropriately respond to patient difficulties and anticipate illness patterns. As a result, cutting-edge and developing technologies are increasingly being used in healthcare. Cloud computing is one of the cutting-edge technologies having significant effects on medical practice, as this quick assessment of it shows.
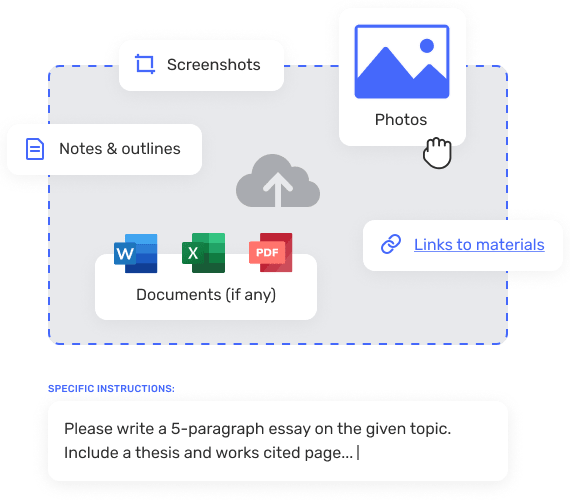
A health care cloud is an example of a computing service used by healthcare providers to store, manage, and back up patient data. In other words, cloud computing is concerned with the internet-based delivery of computer services such as databases, networking, analytics, servers, and storage. Cloud computing, according to Gao et al. (2018), is a technique for improving data storage, management, and processing remotely rather than using regular servers. Cloud computing facilitates the democratization of data and the incorporation of artificial intelligence into ordinary health-care procedures.
Issues and How Cloud Computing Might Work in a Healthcare Setting
Cloud computing allows for the management andin healthcare settings. At a time when health care organizations must deal with massive numbers of electronic health records and big data analytics, cloud computing allows them to keep patient data while avoiding the costly storage associated with physical servers. Cloud computing, according to Dang et al. (2019), is critical for encouraging collaboration among healthcare professionals in order to improve patient care. As a result, its implementation would result in a situation in which health care professionals communicate and collaborate in teams while effortlessly sharing vital patient data. Despite these benefits, there are certain legal issues with cloud computing. The security of patient data is a genuine worry when it comes to cloud computing (Smys & Raj, 2019). Because health care organizations are obligated to follow data portability and security standards, such as the US’s Health Insurance Portability and Accountability Act, there is widespread worry about storing apps and patient data on third-party servers (HIPAA).
Also Read:
Description:
New health care provide an opportunity for advanced registered nurses to use emerging technologies in practice to improve quality and patient outcomes. Research an emerging health care technology that you believe has the potential to overcome current or emerging barriers to care for this assignment.
Emerging Paper
Inefficiency and human errors in medical and health processes such as surgery and other intensive care interventions are major concerns in today’s healthcare practice. Medical errors caused by human factors cause increased delays, limited access to health care services, and higher mortality and morbidity rates. These issues have compelled the development of autonomous and semi-autonomous medical equipment, such as robots, using artificial intelligence. The primary goal of artificial intelligence is to make computers more useful in generating solutions to difficult health-care problems (Secinaro et al., 2021). The goal of this paper is to talk about artificial intelligence as a healthcare technology that has the potential to address new barriers in healthcare delivery.
Because it allows providers to interpret data to diagnose chronic conditions such as diabetes, Alzheimer’s disease, and various types of cancer, artificial intelligence makes computers more important in resolving difficult health-care issues. In the future, using AI for clinical trials will aid the healthcare sector in developing biomarkers to detect various types of conditions such as cancers during the screening process. Data on the coronavirus disease 2019 (COVID-19) pandemic, for example, can be interpreted using AI. The next generation of radiology tools is being developed using artificial intelligence (AI). Brain-computer interfaces, according to studies, can significantly improve the quality of life for patients with terminal conditions such as Alzheimer’s disease, strokes, and people with spinal cord injuries all over the world (Secinaro et al., 2021). Deep learning models can assist in predicting the efficacy of both old and new drugs and treatments on COVID-19. Institutions are utilizing AI to create prototype COVID-19 vaccines and treatments. As a result, AI is an important part of combating the COVID-19 pandemic.
AI has the potential to increase patient access while also improving patient safety and quality. AI interprets data to help health care providers make better decisions and take the best actions to provide the best care while minimizing medical errors. With the addition of more computer-based tools and interventions, many patients, particularly those suffering from terminal conditions such as diabetes and strokes, will be able to access care from remote locations (OECD, 2020). Data from COVID-19 tracing apps and applications like DeepMind demonstrate how artificial intelligence can provide interventions for quality care delivery for patients and health organizations dealing with the pandemic.
Ethical and Legal Issues in Incorporation of
The informatics nurse is critical in information dissemination and the use of health information technologies for effective care delivery and innovation models. The use of artificial intelligence (AI) in health care is an example of an innovative model that providers and organizations are leveraging to improve patient quality care outcomes, particularly during this pandemic period (Pee et al., 2018). As a result, informatics nurses are experts who advise their organizations and help to establish systems that incorporate AI technology for quality care and better services. Nurse informatics’ role is to ensure that facilities that use AI adhere to existing legal protocols and laws, as well as embrace ethical values to protect patient information (Booth et al., 2021). To ensure that AI works for patients and organizations based on the goals and objectives established, nurse informaticists must use the most appropriate channels to provide better software and hardware.
Workflow analysis, human factors, and user-centered design concepts are all important.
Workflow analysis and human factors are critical to the overall success of artificial intelligence in health care. Human factors such as human resource availability ensure that facilities have the necessary abilities and expertise to roll out better technologies to improve care provision. AI should benefit users, particularly patients, rather than just healthcare providers, according to the user-centered design concept (Islam et al., 2021). The ultimate goal in this case should be increased benefits for all stakeholders as a result of the features that AI provides when integrated into the health system and network.
Informatics Nurse’s Role Concerning Artificial Intelligence
The informatics nurse is essential in the dissemination of information and the use of health information technologies for effective care delivery and innovation models. The application of artificial intelligence (AI) in health care is an example of innovative models that providers and organizations are leveraging to improve quality care outcomes for patients, particularly during this pandemic period (Pee et al., 2018). As a result, informatics nurses are experts who advise their organizations and assist in the establishment of systems to incorporate AI technology for quality care and better services. The role of nurse informatics is to ensure that facilities that use AI follow existing legal protocols and laws, as well as embrace ethical values to protect patient information (Booth et al., 2021). Nurse informaticists must use the most appropriate channels to provide better software and hardware to ensure that AI works for patients and organizations based on the goals and objectives established.
Workflow Analysis, Human Factors, and User-Centered Design Concepts Play a Role
Workflow analysis and human factors are critical to artificial intelligence’s overall success in health care. The workflow analysis allows providers to identify areas that require improvement and can benefit from AI technologies, while human factors such as human resource availability ensure that facilities have the necessary abilities and expertise to roll out better technologies to improve care provision. According to the user-centered design concept, AI should benefit users, particularly patients, rather than just healthcare providers (Islam et al., 2021). The ultimate goal in this case should be increased benefits for all stakeholders as a result of the features that AI provides when integrated into the health system and network.
Conclusion
are essential to enhancing quality care and patient outcomes. These technologies like artificial intelligence are revolutionizing the overall care experience for patients and helping nurse practitioners and other professionals to offer better interventions and enhance accessibility. Informatics nurses have a duty to ensure that they help in the implementation of artificial intelligence in their practice settings to enhance overall care delivery as innovative models in healthcare.
References
Booth, R., Strudwick, G., McMurray, J., Chan, R., Cotton, K., & Cooke, S. (2021). The Future of
Nursing Informatics in a Digitally-Enabled World. In Introduction to Nursing Informatics (pp. 395-417). Springer, Cham.
Islam, M., Poly, T., Alsinglawi, B., Lin, M., Hsu, M. and Li, Y. (2021). A State-of-the-Art
Survey on Artificial Intelligence to Fight COVID-19. Journal of Clinical Medicine, 10(9), p.1961. https://www.mdpi.com/2077-0383/10/9/1961/htm
Organization for Economic Co-operation and Development (OECD) (2020). OECD Policy
Responses to Coronavirus (COVID-19): Using artificial intelligence to help combat COVID-19. https://www.oecd.org/coronavirus/policy-responses/using-artificial-intelligence-to-help-combat-covid-19-ae4c5c21/
Pee, L. G., Pan, S. L., & Cui, L. (2019). Artificial intelligence in healthcare robots: A social
informatics study of knowledge embodiment. Journal of the Association for Information Science and Technology, 70(4), 351-369.
Secinaro, S., Calandra, D., Secinaro, A., Muthurangu, V., & Biancone, P. (2021). The role of
artificial intelligence in healthcare: a structured literature review. BMC Medical Informatics and Decision Making, 21(1), 1-23. DOI: https://doi.org/10.1186/s12911-021-01488-9
Re: Topic 5 DQ 1
The Mayo Clinic remains one of the more innovative models of care to date. In response to the rapidly changing healthcare scene, the Mayo Clinic launched their Mayo Clinic Care Network (MCCN) in 2011 (Wald et al., 2018) and it has only continued to grow. The Mayo Clinic is considered innovative due to their formal and widespread use of collaboration that spans continents (Wald et al., 2018). As of 2017, the MCCN had 45 partners, spanning across 35 US states and including the Philippines, Mexico, Puerto Rico, Singapore, and the United Arab Emirates (Wald et al., 2018). International locations is not what makes the MCCN innovative, however. It is considered innovative because providers and healthcare teams can collaborate globally on a case, enabling an MCCN physician to utilize their best resources anywhere in the world. Providers can eConsult an expert for a case without that expert having to physically relocate or force the patient to seek care elsewhere (Wald et al., 2018). Providers can also participate in eBoards, where experts from across the MCCN come together to discuss particular cases on a larger scale (Wald et al., 2018). The Ask Mayo Expert feature brings Mayo Clinic knowledge right into the hands of the patient via internet, enabling patients to glean trusted information when and where they need it (Wald et al., 2018). By using technology to bring teams and patients together, the cost of travel alone is nearly reduced to zero. All of these pieces come together to form a large network of highly collaborative experts with mobilized resources, thus furthering the ability to provide state of the art care when and where the patient needs it most.
Wald, J. T., Lowery-Schrandt, S., Hayes, D. L., & Kotsenas, A. L. (2018). Mayo Clinic Care Network: a collaborative health care model. Journal of the American College of Radiology, 15(1PB), 167-172. https://www.jacr.org/article/S1546-1440(17)31186-9/pdf
RESPOND HERE (150 W0RDS, 2 REFERENCES)
Hello Ali,
I do agree with you that among one of the healthcare organizations that have successfully incorporated innovations in technology to increase collaboration is Mayo Clinic. This giant healthcare system has well established networks in over 140 countries and 50 states in the US. This extensive coverage with an annual patient load going to over one million, it calls on improved technological innovations that promote timely and effective care to the patients. Among the 65,000 employers of the clinic, there are various specialties that work in multidisciplinary team’s collaboration approach to deliver quality care. Dr. William. J. Mayo, the founder of the organization, had the greater vision on how clinical collaboration would be the most efficient and effective way to deliver quality and timely care to the patients (Taberna et al., 2020). “The best interest of the patient is the only interest to be considered, and in order that the sick may have the benefit of advancing knowledge, union of forces is necessary.” — Dr. William J. Mayo, 1910 (“Mayo Clinic Care Network – About Us – Mayo Clinic, 2019”).
References
Mayo Clinic Care Network – About Us – Mayo Clinic. (2019). Mayoclinic.org;
Taberna, M., Gil Moncayo, F., Jané-Salas, E., Antonio, M., Arribas, L., Vilajosana, E., Peralvez Torres, E., & Mesía, R. (2020). The Multidisciplinary Team (MDT) Approach and Quality of Care. Frontiers in Oncology, 10(85).
Re: Topic 5 DQ 2
Accountable Care Organizations (ACOs) are composed of physician groups, hospitals, and other professions that provide health care to provide quality, systematic care to Medicare patients. ACOs tend to reduce health care costs through the coordination of care that eliminates overlapping or duplicated methods of care. All members must collaborate to create a smooth transition in care to achieve maximum reimbursement. ACO members are driven to create innovations that improve care and reduce costs to receive full reimbursement from Medicare. Within this idea, many programs have been created to provide optimal patient outcomes. The total joint replacement initiative seeks to optimize patients, reduce the recovery period, minimize complications, and decrease health care costs. The joint replacement center addresses areas of nutrition, wound healing, deep vein thrombosis prophylaxis, pain control, medications for nausea, early ambulation, and physical and occupational therapy. These areas are addressed to prevent complications and hospital readmissions. Perioperative service at the hospital I work at has established clinical pathways that utilize evidence-based practices for optimal care. This is a beneficial scenario for patients. The nation’s health care personnel must collaborate to develop innovative ideas to maximize patient outcomes while reducing costs. D’Aunno et al. (2018) identify several factors of high-performing ACOs. These components are physician collaboration with hospitals, optimal physician group practice before ACO adoption, effective physician leaders focused on high-quality care, adept use of information systems, constructive feedback to physicians, and care coordinators (D’Aunno et al., 2018). Addressing these areas in an ACO will assist in providing optimal care with resultant reimbursement.
References
D’Aunno, T., Broffman, L., Sparer, M., & Kumar, S. R. (2018). Factors that distinguish high-performing accountable care organizations in the medicare shared savings program. Health Services Research, 53(1), 120–137.
RESPOND HERE (150 W0RDS, 2 REFERENCES)
MELINA
Re: Topic 5 DQ 2
McAlearney et al. (2018) states “Across the health care landscape in the United States, momentum is shifting away from volume-based care and building toward value-based care most often interpreted as a function of reducing cost while simultaneously improving quality.” (p. 4767) Accountable care organizations involve organizational partnerships for the purpose of coordinating patient care across the health care continuum to improve health outcomes. ACOs focus on outcomes as this is what drives reimbursement. Improving care while reducing costs may require innovative use of existing resources and use of innovative means of achieving treatment goals. Looking at the end result is a straightforward way of quantifying the efficacy, and quality of the services delivered by participating providers. 81% of ACOs involve new partnerships between independent health care organizations whose providers are motivated to partner for resource complementarity, risk reduction, and legislative requirements, and are using a variety of formal and informal accountability mechanisms.” (Lewis et al., 2017, p. 25) Value-based reimbursement creates the incentive for ACOs to manage patient care across health care settings, requiring improved care coordination among providers. These efforts reduce unnecessary health care utilization, improve patient outcomes, and reduce health care spending. (Agarwal & Werner, 2018)
References
Agarwal, D., & Werner, R. M. (2018). Effect of Hospital and Post-Acute Care Provider Participation in Accountable Care Organizations on Patient Outcomes and Medicare Spending. Health Services Research, 53(6), 5035–5056.
Lewis, V. A., Tierney, K. I., Colla, C. H., & Shortell, S. M. (2017). The new frontier of strategic alliances in health care: New partnerships under accountable care organizations. Social Science & Medicine (1982), 190, 1–10. https://doi-org.lopes.idm.oclc.org/10.1016/j.socscimed.2017.04.054
McAlearney, A. S., Walker, D. M., & Hefner, J. L. (2018). Moving Organizational Culture from Volume to Value: A Qualitative Analysis of Private Sector Accountable Care Organization Development. Health Services Research, 53(6), 4767–4788. https://doi-org.lopes.idm.oclc.org/10.1111/1475-6773.13012
Re: Topic 6 DQ 2
Electronic Medical Records (EMRs) and Electronic Health Records (EHRs) are not the same. Though they are only one letter apart, EMRs and EHRs actually have very different functions. Both are digital programs that house patient information, thus greatly decreasing the reliance on physical paper copies. Both can be used for data tracking and as a tool to ensure patients are receiving proper preventative care, such as immunizations and screenings (Garrett & Seidman, 2011).
An EMR is a digitized version of a patient’s medical chart from one specific facility. It includes provider notes, diagnoses, and treatments, all of which occurred at that one clinic in particular (Garrett & Seidman, 2011). EMRs are not easily transferrable to other facilities, however, and often may need to be physically printed out for the information to be shared outside of the clinic/facility (Garrett & Seidman, 2011).
While an EMR focuses on the “medical” aspect, an EHR focuses on “health” as a whole, which is a much broader view (Garrett & Seidman, 2011). EHRs can do everything an EMR can do, and more. They can house information not just from one specific clinic or facility, but from all providers a patient may see, providing a holistic look at the patient’s care as a whole (Garrett & Seidman, 2011). Information can be shared between facilities without the cumbersome process of printing and faxing, providers can collaborate with confidence knowing they’re seeing the same information, and the EHR moves with the patient wherever they go (Garrett & Seidman, 2011).
There are more than 800 certified commercial EHRs for inpatient facilities (DeNisco & Barker, 2016). A commonly used EHR is Epic, which is what my hospital system just switched to, from Cerner/ORCA. We made the switch to Epic for our inpatient facilities because our outpatient clinics were already using it, and Epic and Cerner did not share information with each other. While switching to Epic was not a smooth transition and we are still working through ongoing issues months later, it was a move made in the name of interoperability and patient quality and access to care. Having out outpatient and inpatient systems talk to each other provides invaluable information when a patient finds themselves inpatient. Providers and care teams can be confident that they see the holistic picture of the patient’s medical care, instead of having to fill in holes in records and spend time piecing together the history.
DeNisco, S.M., & Barker, A.M. (2016). Advanced practice nursing. Essential knowledge for the profession (3rd ed.). Burlington, MA: Jones & Bartlett Learning.
Garrett, P., & Seidman, J. (2011). EMR vs EHR—what is the difference? The Office of the National Coordinator for Health Information Technology.
Refer to the Topic 6 materials for samples and resources to help you construct your brief.
You are required to cite three to five sources to complete this assignment. Sources must be published within the last 5 years and appropriate for the assignment criteria and nursing content.
While APA style is not required for the body of this assignment, solid academic writing is expected, and documentation of sources should be presented using APA formatting guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion. Emerging Technology Brief NUR 514
You are required to submit this assignment to LopesWrite. Refer to the LopesWrite Technical Support articles for assistance.
Emerging Technology Brief
Health care innovations provide advanced registered nurses the opportunity to use emerging technologies in practice to enhance quality patient outcomes. Electronic health records (EHRs) as an emerging technology, provides nurses and other health care providers with increased benefits in providing care for patients in their clinical settings. Electronic health records do more than collecting and storing patient information (McBride et al., 2018). Increasingly, these records not only compute but also communicate the data and provide insights that make a difference in the care provision and treatment process. As such, this essay describes electronic health records as an emerging technology whose use continues to expand in health care provision.
Electronic Health Records: Overview, Purpose, and Function in Health Care Setting
A patient’s paper chart and information are digitized in an electronic health record (EHR). EHRs are patient-centered records that make data available to authorized users instantly and securely. An EHR system is designed to store standard clinical data collected in a provider’s office and can provide a comprehensive view of a patient’s care (Evans, 2016). EHRs are a critical component of health IT because they allow nurses to access evidence-based tools to make decisions about a patient’s care. EHRs also automate and streamline the workflow of providers.
These systems also store a patient’s medical history, medications, diagnoses, and pertinent information on allergies, laboratory results, and treatment plans. Again, data shared in an EHR system can assist clinicians in selecting the best medication for allergy patients. Nurses use electronic health records to make more informed decisions about the type of care to give to individual patients.
The passage of the Health Information Technology for Economic and Clinical Health Act (HITECH) in 2009 increased the use of electronic health records (EHRs) as a means of documenting health care delivery in acute care settings and guiding care decisions made by nurses based on this information and consultation with other providers, particularly physicians (Jenkins et al., 2018). McBride et al. (2018) assert in their study that electronic health records in health settings have increased with a saturation rate of more than 90% as a critical aspect of improving care outcomes and patient safety.
Ethical or Legal Issues
The incorporation of electronic health records presents ethical and even legal issues that should be addressed based on existing legal and ethical frameworks by regulatory agencies and professional associations like the American Nurses Association (ANA) (Jenkins et al., 2018). Studies show that in many aspects, meaningful use of EHRs improves care, and nurses experience increased satisfaction by applying the technology (Robin, 2016). However, mounting evidence shows that the same systems can result in unintended impacts with implications on patient safety and contribute to the provider’s moral distress. For instance, nurses and clinical teams encounter usability complications that present ethical issues and need ethical decision-making approaches.
Among the ethical issues concerning EHRs is patient privacy and security risks. As required by Health Insurance Portability and Accountability Act (HIPAA), a breach of confidentiality can lead to legal challenges since providers are not required to share private information concerning a patient (Balestra, 2017). The risk of a breach happening is higher when using EHR systems. Therefore, nurse practitioners must be keen on avoiding unauthorized access to patient information.
EHRs in Improving Access to Care and Promoting Safety and Quality
At the core of EHR systems is to enhance quality outcomes and access to health through easy information availability and sharing with other providers (Jenkins et al., 2018). Further, EHRs are critical in patient safety since they contain information concerning medications and history for effective decision-making and adherence to specific rules to reduce potential medication errors.
Conclusion
The use of EHRs as health and medical technologies is an accepted standard that has led to better decision making, enhanced quality outcomes, and increased patient engagement in their treatment process. As such, providers should leverage on the EHRs to improve quality, make better and evidence-based decisions and interventions, and engage patients with a view of improving care delivery.
Current Law
Laws related to the use of AI focus on the impact of the technology on safety to the patients receiving the care. According to Yu, Beam & Kohane (2018), robots should not be used as replacement for human doctors. In essence the machines should guide decisions in care but not used singly without the intervention of a trained clinician. However, Mamoshina et al. (2018) suggest that the use of AI for diagnosis is a medical malpractice law as it violates the standards of care and due diligence required to realize a standard of care. In essence, the AI machines are likely to yield overwhelming legal as well as ethical pressure that may not be understood by human doctors. Preliminary evaluation in the use of AI indicates that the technology may be compounded by lack of transparency which can compromise the quality of care.
Background
Organization policy: Improved efficiency by the use of latest technology to improve care.
Action:
- The use of robots for surgical procedures
- Use of AI for electronic health records
- Implementation of AI to dispense prescription drugs
Evidence-base: Robots have been successfully used to conduct surgeries and as the procedures are less invasive due to use of small incision blades (Verghese, Shah & Harrington, 2018).
Regulatory Framework:
- Use of robots is accepted if it guarantees safety to patients.
- Use of AI adheres to the ethical practice in standard of care for patients
References
Jha, S., & Topol, E. J. (2016). Adapting to artificial intelligence: radiologists and pathologists as information specialists. Jama, 316(22), 2353-2354.
Mamoshina, P., Ojomoko, L., Yanovich, Y., Ostrovski, A., Botezatu, A., Prikhodko, P., … & Ogu, I. O. (2018). Converging blockchain and next-generation artificial intelligence technologies to decentralize and accelerate biomedical research and healthcare. Oncotarget, 9(5), 5665.
Verghese, A., Shah, N. H., & Harrington, R. A. (2018). What this computer needs is a physician: humanism and artificial intelligence. Jama, 319(1), 19-20.
Yu, K. H., Beam, A. L., & Kohane, I. S. (2018). Artificial intelligence in healthcare. Nature biomedical engineering, 2(10), 719.
The Emerging Technology, Its Purpose, and How it Would Function in a Health Care Setting, Including Any Ethical or Legal Issues
EMRs (Electronic Medical Records) and EHRs (Electronic Health Records) are not the same thing. Despite the fact that they are only one letter apart, EMRs and EHRs serve very different purposes. Both are digital programs that store patient information, reducing the need for physical paper copies. Both can be used to track data and as a tool to ensure that patients receive necessary preventative care, such as immunizations and screenings (Garrett & Seidman, 2011).
An electronic medical record (EMR) is a digitized version of a patient’s medical chart from a single facility. It contains provider notes, diagnoses, and treatments that all occurred at that specific clinic (Garrett & Seidman, 2011). However, EMRs are not easily transferable to other facilities and must often be physically printed out for information to be shared outside of the clinic/facility (Garrett & Seidman, 2011).
While an EMR is concerned with the “medical” aspect, an EHR is concerned with “health” as a whole, which is a much broader perspective (Garrett & Seidman, 2011). EHRs can perform all of the functions of an EMR and more. They can store information not just from one clinic or facility, but from all providers a patient may visit, providing a comprehensive view of the patient’s care as a whole (Garrett & Seidman, 2011). Information can be shared between facilities without the time-consuming process of printing and faxing, providers can collaborate confidently knowing they’re seeing the same data, and the EHR follows the patient wherever they go (Garrett & Seidman, 2011).
There are over 800 commercially certified EHRs for inpatient facilities (DeNisco & Barker, 2016). Epic is a popular EHR, and my hospital system recently switched from Cerner/ORCA to Epic. We switched to Epic for our inpatient facilities because our outpatient clinics already used it, and Epic and Cerner did not share information. While the transition to Epic was not easy, and we are still dealing with issues months later, it was a decision made in the name of interoperability, patient quality, and access to care. When a patient becomes a patient, having our outpatient and inpatient systems communicate with one another provides invaluable information. Instead of having to fill in gaps in records and spend time piecing together the history, providers and care teams can be confident that they see the whole picture of the patient’s medical care.
Writing an Issue Brief
The issue brief is a short, written document that:
- states the issue for consideration;
- indicates a recommendation for action;
- provides supporting information relevant to the issue and recommendation;
- lists references for the supporting information and other resources as necessary; and provides contact information.
To be effective the length of an issue brief should be no more than two pages (front and back of one sheet of paper). That is why they are sometimes referred to as one-pagers.
If the issue brief is to be used among members of an organization the information presented in the issue brief should be consistent with and reflect any organizational policy or agenda.
The information presented in an issue brief can be assembled by using the information used in the development of an organizations advocacy agenda.
The Framework of an Issue Brief
Issue
State the issue for consideration. Briefly state what is important to you in the context of a current public policy issue and the relevance of the issue to your intended audience.
Recommendation
State the action you seek in connection with the above-stated issue. The recommendation may indicate the continuation, elimination, or amending of the issue.
Current Law
List any current law or regulatory framework that authorizes or supports the issue.
Background
Provide supporting information relevant to the issue and recommendation:
- List any organizational policy that supports or is relevant to the issue;
- List the actions you employ or activities in which you engage in that demonstrate the importance of that issue to you;
- List the current evidence-base that supports your actions or activities or suggests that these actions or activities lead to a given outcome; and
- List the evidence-base used to establish the laws or regulatory framework listed above.
References/Resources
- List the appropriate citations for the evidence-base you provide within the issue brief.
- List any additional resources that you deem important to support your recommendation.
Contact Information
List the individuals the recipient of the issue brief can contact for more information about the issue.
Topic 6 DQ 1
In what ways can informatics help health care providers overcome current or emerging barriers to care and increase access to safe, quality health care? Include a discussion of the value and challenges of clinical provider order entry (CPOE) and clinical decision support systems (CDSS) in providing safe patient care in your response.
Nursing informatics refers to a “specialty that combines nursing science with numerous information and systematic sciences to identify, define, manage, and communicate data, information, knowledge, and wisdom in nursing practice” (McGonigle & Mastrian, 2018). Nursing informatics help improves nursing practice and enhances the quality of care. On the other hand, health informatics is the acquisition, storage, retrieval, dissemination of healthcare information to promote quality patient care” (USF Health, 2020). Health Informatics fosters safe patient care as it allows healthcare providers to access patient data. It also encourages better collaboration among a patient’s numerous healthcare providers. There are many ways that health informatics improves patient care. One way is maintained medical records: the development of electronic health records (EHR) has made the management of patient records convenient and safe because healthcare providers can access the data easily. The second way is the reduced cost. EHR helps reduce medication errors and prevents replication of tests and labs because providers can check the database to ensure that the intended tests have not been completed recently, thus reducing the cost. The third way that EHR improves the quality of care is it lessens trial and error. With EHR providers, and pharmacists can easily reconcile medications, therefore, reducing medication interactions, allergic reactions due to polypharmacy. Patients can easily self-manage their illnesses. The EHR allows patients to access their health information easily.
Utilizing CPOE helps improve patient care as it is efficient, cost-effective, and prevents medical errors. With the CPOE, the computers remind the providers “what to do, what they already know how to do, and what they want to do, in a manner that makes it easy to implement, resulting in an efficacious computerized decision support system”(Kroth, 2016). For instance, CPOE auto-populates order sets for the providers which, are efficient and effective.
References
McGonigle, D., Mastrian, K. (2018). History and Evolution of Nursing Informatics. Nursing Informatics and the Foundation of Knowledge (4th ed., pp. 104-116). Burlington, MA: Jones & Bartlett Learning. doi:https://viewer.gcu.edu/mQmVy7
Kroth, P. J. (2016). Health Information Technology. In DeNisco. M. S., Barker, A. M. (Eds.), Advanced Practice Nursing: Essential Knowledge for the Profession (3rd ed., pp. 323-348). Burlington, MA: Jones & Bartlett Learning. doi:https://viewer.gcu.edu/Tce3cz
USF Health, Morsani College of Medicine (2020). What is Health Informatics? Retrieved December 16, 2020, from https://www.usfhealthonline.com/resources/key-concepts/what-is-health-informatics/
Topic 6 DQ 2
Differentiate between EMRs and EHRs. Discuss the importance of interoperability in relationship to both types of records and to how the EMR and EHR improve quality and access to care.